The battle against cancer is one of the greatest challenges in modern medicine. Despite advancements in treatment, many cancers are diagnosed at advanced stages, when survival rates are still low. Early detection is key to improving patient outcomes, yet many cancers, such as pancreatic cancer, remain difficult to diagnose at an early stage.
Fortunately, artificial intelligence (AI) and machine learning (ML) are revolutionizing cancer diagnostics, offering the potential to detect cancer earlier, identify molecular subtypes, and provide more personalized treatment options. Through the use of AI-driven diagnostic tools, researchers are making significant strides in ensuring that cancer can be detected more effectively and treated with greater precision.
Key Takeaways
Artificial intelligence (AI) is revolutionizing pancreatic cancer care by enabling early diagnosis, accurate classification, and personalized treatment plans.
- AI-driven diagnostic tools can detect pancreatic cancer earlier and classify it into molecular subtypes with high accuracy, improving patient outcomes.
- AI-based cancer diagnostics can provide more timely treatment decisions by analyzing routine hematoxylin and eosin (H&E) stained slides in a matter of hours.
- AI’s role in personalized cancer treatment involves tailoring therapies to an individual’s genetic or molecular tumor profile, guiding treatment plans, and connecting patients to clinical trials targeting their specific cancer type.
AI in pancreatic cancer subtyping
Pancreatic cancer, specifically pancreatic ductal adenocarcinoma (PDAC), is one of the most aggressive and deadly cancers. It has recently surpassed breast cancer as the third leading cause of cancer-related deaths in the United States and Canada.
PDAC is notoriously difficult to diagnose at early stages, and the survival rate for those diagnosed with metastatic disease is alarmingly low. Surgery, while potentially curative, is only effective in approximately 20% of cases, and the overall five-year survival rate remains at just 20%. By the time patients are diagnosed, most have already developed metastatic disease, further reducing treatment options and survival rates.
Researchers are focusing on improving PDAC diagnostics through AI, to detect the cancer earlier and classify it more accurately. A recent study published in The American Journal of Pathology demonstrated that deep learning models can be used to classify PDAC into molecular subtypes, providing a faster, more cost-effective alternative to traditional diagnostic methods.
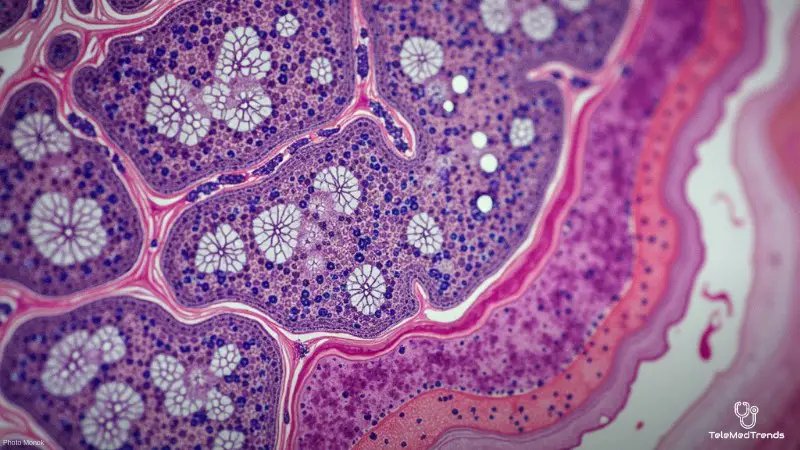
The study used whole-slide pathology images to train AI models, achieving an impressive accuracy rate of 96.19% in identifying two major PDAC subtypes: basal-like and classical. These subtypes have different clinical behaviors and treatment responses, making accurate classification critical for effective treatment planning.
Challenges in pancreatic cancer diagnostics
Traditionally, the diagnosis of pancreatic cancer has relied on genomic sequencing methods, which are expensive and time-consuming. Genomic sequencing often requires large tissue samples, which can be difficult to obtain, given the pancreas’s deep anatomical location. This has made it challenging to diagnose PDAC early enough to make a difference in treatment.
The AI tool developed in the study provides a solution by analyzing routine hematoxylin and eosin (H&E) stained slides, which are a standard and widely available method for tissue staining in pathology labs. The deep learning models trained on these slides were able to identify PDAC molecular subtypes with high accuracy, providing a faster, more affordable diagnostic approach.
The benefit of using AI for PDAC diagnostics lies not only in its cost-effectiveness but also in its speed. Traditional molecular profiling of PDAC can take anywhere from 19 to 52 days to produce results, which is a critical issue for a rapidly progressing cancer.
In contrast, the AI tool can analyze H&E slides in a matter of hours, significantly reducing turnaround times and enabling clinicians to make more timely treatment decisions. This is particularly important for PDAC, as the disease’s aggressive nature necessitates swift action to determine eligibility for targeted therapies or clinical trials.
AI’s role in personalized cancer treatment
AI-based cancer diagnostics can enable personalized treatment by tailoring therapies to an individual’s genetic or molecular tumor profile. Traditionally, treatments were based on general cancer categories, but AI tools allow doctors to customize care based on specific cancer subtypes.
For pancreatic cancer, identifying subtypes like basal-like and classical can guide treatment. The basal-like subtype may resist certain treatments, while the classical subtype may respond better. Early detection of these subtypes helps doctors personalize treatment plans and connect patients to clinical trials targeting their specific cancer type.
The Role of AI in Predicting Cancer Progression
AI does not only help in identifying cancer subtypes but also plays a key role in predicting how a cancer will behave over time. Machine learning models can analyze vast amounts of patient data, including genetic profiles, medical histories, and imaging studies, to predict how an individual’s cancer will progress.
This can help clinicians anticipate how a tumor might respond to treatment, whether it is likely to metastasize, and what the overall prognosis might be. Such predictive capabilities can aid in developing more effective treatment strategies and improving patient outcomes.
Moreover, AI can also help identify early warning signs of recurrence. For example, AI models can analyze follow-up scans and lab results to detect subtle changes in tumor size or molecular markers that might indicate the cancer is coming back. Early detection of recurrence is critical for implementing timely interventions that can prevent the cancer from progressing further.
AI and other diagnostic technologies
AI is expected to enhance cancer detection and treatment by integrating with technologies like liquid biopsy, which analyzes blood samples for genetic mutations or biomarkers. Liquid biopsy offers a non-invasive method to monitor cancer and track treatment, while AI can help interpret complex data, uncovering patterns human clinicians may miss.
Advanced imaging techniques, like MRI, CT scans, and PET scans, provide insights into tumors, but detecting subtle early-stage changes can be difficult. AI-powered imaging analysis can automate interpretation, improving accuracy and speed. By combining AI with liquid biopsy and advanced imaging, healthcare providers can develop a more effective system for early cancer detection.
Enhancing accessibility and overcoming barriers
While AI shows great promise in improving cancer diagnosis and treatment, several challenges must be addressed for widespread clinical adoption. A key challenge is ensuring AI tools are accessible and effective in diverse healthcare settings, including those with limited resources.
Many AI systems are still in the research phase, and scaling them up for widespread use will take time. For AI to be truly transformative, it must become part of routine clinical practice, with healthcare professionals trained and infrastructure ready to support these technologies.
Data privacy and security are also major concerns. AI systems require large amounts of patient data to train algorithms, raising questions about how data is collected, stored, and used. Safeguarding patient confidentiality will be essential to gaining trust and ensuring ethical AI use in healthcare.
Additionally, addressing biases in AI algorithms is critical. If AI models are trained on non-diverse datasets, they may not be effective for certain populations. Researchers must ensure AI models are trained on datasets representing diverse patient demographics.
Despite these challenges, AI’s future in cancer diagnostics is bright. Rapid progress is being made in developing tools to detect cancers like pancreatic cancer earlier, classify them accurately, and offer personalized treatment plans. These advancements, combined with AI’s integration with other diagnostic technologies, could revolutionize cancer diagnosis and treatment, improving early detection, survival rates, and quality of life for patients.
Expanding AI’s role in cancer care
Looking ahead, the role of AI in cancer care will continue to expand. As more molecular subtypes of various cancers are discovered, AI will play a pivotal role in identifying these subtypes and guiding treatment decisions. With the potential to predict cancer progression, monitor treatment response, and even detect recurrence, AI will help clinicians provide more personalized and effective care.
However, for AI to truly fulfill its potential, it must be integrated into healthcare systems, ensuring that patients, regardless of their location or socioeconomic status, have access to the latest advancements in cancer diagnostics and treatment.
By harnessing the power of AI, we are entering a new era of cancer care—one that prioritizes early detection, personalized treatment, and better outcomes for patients. The future of cancer diagnostics and treatment is undoubtedly brighter, thanks to the innovative capabilities of AI.